What follows is not intended as a chastisement of anybody. People can say what they want, and, on top of it, the quotations that are given below are more or less true. The only point is to invite researchers who write papers about schizophrenia (and there are a lot of you!), as well as those who edit them, to consider what patients might take away from the first few sentences of your article. Yes patients do read them.
(One might also ask, as an editor: Is it really necessary to begin with these points? Does the target audience of, say, The Lancet Psychiatry, or the American Journal of Psychiatry, or Schizophrenia Bulletin, really need to be told that “schizophrenia is kinda rough”? Again, and again, and again? Why the compulsion to repeat this particular point ad nauseum?)
(In case it isn’t clear, the formatting and tone of the next three paragraphs is tongue-in-cheek—that intention doesn’t always come across clearly on the internet.)
Method: The author searched for “schizophrenia treatment” in Google Scholar, limited to publications from 2024. The first 30 results were included in the analysis. (In some cases it turned out that the actual date of publication was 2025; these results were included.)
Result: Thematic analysis of opening sentences revealed several connected themes, including: (1) schizophrenia (SCZ) can make life difficult; (2) SCZ is often a lifelong condition; (3) SCZ creates a significant burden on others; (4) existing treatments for SCZ aren’t great.
Discussion: What will patients come away thinking about themselves, their prognosis, their doctor, their proposed treatment, their burden on others?
Not every article begins in this fashion. Here are some, from the 30 examined, that do.
“Schizophrenia is a severe psychiatric disorder with significant variance and heterogeneity in symptom profile, social functioning, treatment response, and clinical outcome.” [1]
“Schizophrenia affects approximately 0·7% of the global population during their lifetime, including 0·32% of the population at any one time, and imposes a significant health-care burden worldwide.” [2]
“Schizophrenia is a severe mental illness with onset in late adolescence or early adulthood. It is associated with significant impairment across multiple cognitive and behavioral domains.” [3]
“Characterized by positive, negative, and cognitive symptoms (Millgate et al., 2022), patients with TRS [treatment resistant schizophrenia] have substantial functional impairment, lower quality of life, higher suicide risk, higher substance abuse, and higher social costs than patients without TRS.” [4] (This sentence is the second, not first.)
“Schizophrenia (SZ) is a chronic, severe, and disabling mental disorder with approximately 1% of the general population globally affected and with heritability estimated at up to 80% (Cardno and Gottesman, 2000; Sullivan et al., 2003; Keller et al., 2013; Wright et al., 2013). This major psychotic disorder has late adolescence or early adulthood onset and complex clinical symptoms related to neurocognitive and neurophysiological dysfunction. The disease is characterized by positive symptoms (such as changes in behavior or thoughts, including delusions and hallucinations), negative symptoms (such as apathy, anhedonia, and social withdrawal), and cognitive impairments (Cassoli et al., 2016; Qin et al., 2017). The decreased attention levels, working memory, verbal learning and memory, reasoning and problem solving, speed of processing, and executive functioning typical of this condition result in low quality of social relationships, declining self-care skills, and reduced capacity for independent living (Marder, 2006; Green et al., 2015; DeTore et al., 2019).” [5]
“The complexity and heterogeneity of symptoms present in individuals living with schizophrenia have contributed to challenges in effectively treating this chronic and disabling neuropsychiatric syndrome. In fact, even with available treatments, many, if not most, people living with schizophrenia remain disabled by one or more of their symptoms for their entire lives.” [6]
“Schizophrenia Spectrum Disorders (SSD) represent severe and often debilitating mental disorders that frequently have a consistent negative impact on people’s functioning and real-world outcomes.” [7]
“Schizophrenia is a chronic and serious mental illness affecting almost 24 million people worldwide, characterised by positive, negative, affective, and cognitive symptoms leading to serious functional disability.” [8]
“Schizophrenia is a disabling and heterogeneous disorder, affecting around 1% of the general population worldwide.” [9]
“Schizophrenia is a leading cause of global disability that affects about 1% of people and typically develops in early adulthood.” The next paragraph begins: “Schizophrenia carries a substantial financial and societal cost owing to its onset in early adulthood, social and occupational impairment, and overall reduced life expectancy.” [10]
“Schizophrenia is a major mental disorder and a leading cause of chronic disability.” [11]
“Schizophrenia is a devastating psychiatric disorder that has a detrimental impact on a considerable population worldwide, severely limiting psychosocial functioning and imposing a significant burden on society.” [12]
“Schizophrenia is a leading cause of global disease burden. Current drug treatments are associated with significant side effects and have limited efficacy for many patients.” [13]
“Schizophrenia is a debilitating mental illness believed to be present in approximately 0.5% of the global population; the 2016 Global Burden of Disease Study ranked schizophrenia as the 12th most disabling disorder.” [14]
“For approximately 20%-30% of individuals with schizophrenia, the illness does not respond to two or more adequate trials, in terms of dose and duration, of first-line antipsychotic medications. This condition is clinically defined as treatment-resistant schizophrenia (TRS), which is linked to significantly diminished quality of life for patients and substantially higher socioeconomic costs compared to non-TRS, imposing a considerable burden on both individuals and society.” [15]
“Schizophrenia is a severe mental disorder characterized by a chronic course, marked impairments in social and vocational functioning, and a generally poor prognosis, often imposing a heavy burden on families and society.” [16]
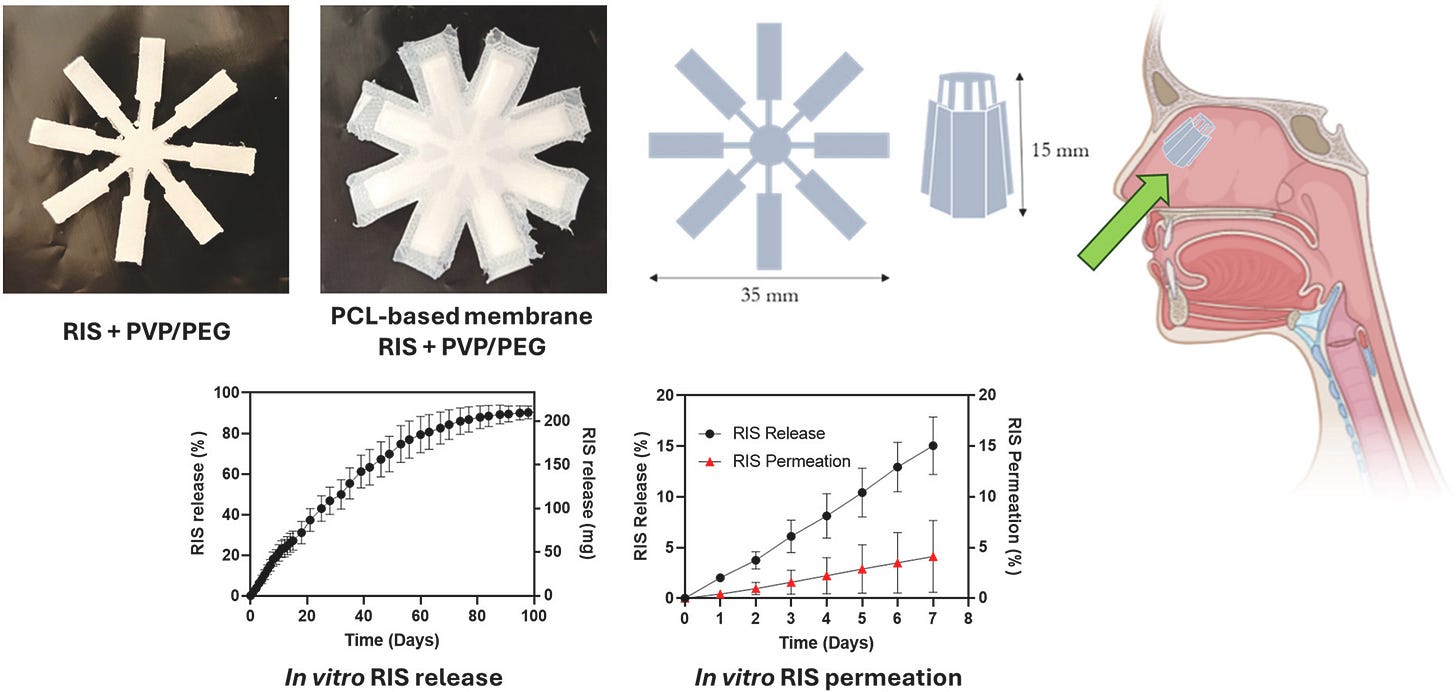
Finally, here are two that caught my attention because they don’t quite fit the mold. The first is just an image (the ‘graphical abstract’ for the article) that I cannot get out of my head:
And last—refreshingly!—is an article [18] that, while it does begin a little bit similarly to the others (“Schizophrenia is a complex and chronic mental illness”), quickly pivots to focus on “overall recovery of individuals with schizophrenia and their reintegration into normal life”, not by shoving objects into your sinuses, but through exercise. Yay for exercise!
I’m going for a bike ride.
References (not full, just enough to find the article for those who want)
[1] Lányi et al. 2024. Schizophrenia Research 264:327–335.
[2] McCutcheon et al. 2025. The Lancet Psychiatry 12(5):384–394.
[3] Crump et al. 2024. Expert Review of Neurotherapeutics 24(8):727–733.
[4] Chen et al. 2024. Progress in Neuro-Psychopharmacology and Biological Psychiatry 130:110926.
[5] Martinez and Peplow. 2024. Neural Regeneration Research 19(7):1523–1531.
[6] Paul et al. 2024. Biological Psychiatry 96(8):627–637.
[7] Vita, Nibbio, and Barlati. 2024. Schizophrenia Bulletin Open sgae013.
[8] Salahuddin et al. 2024. Lancet Psychiatry 11:545–553.
[9] Martini et al. 2024. Eur Arch Psychiatry Clin Neurosci 274:1473–1481.
[10] Howes et al. 2024. Nat Rev Neurol 20:22–35.
[11] Javitt. 2025. Am J Psychiatry 182:3.
[12] Wang et al. BMC Psychiatry 24:53.
[13] Howes et al. 2024. Biological Psychiatry 96(8):638–650.
[14] Tsugawa et al. Schizophrenia Bulletin 50(2):382–392.
[15] Cedeno et al. Cureus 16(6):e62625.
[16] Han et al. 2025. Translational Psychiatry 15:210.
[17] Utomo et al. 2024. Journal of Drug Delivery Science and Technology 99:105973.
[18] Guo et al. 2024. Schizophrenia 10:2.


I love that you did your own (pseudo) research study on this! It’s quite interesting that most researchers feel the need to write some version of “schizophrenia is bad” to start their papers. Perhaps if more creativity and humility was allowed in scientific academia, they might start by humanizing people with the disorder instead.
Nice post, yeah, I've talked about this in the case of autism. It's almost like a rhetorical tick or ritual that every scholarly article on autism has to start with the sentence "Autism is a devastating disease" in the first paragraph, regardless of what comes next.
Given the wild over representation of autistic people in science and academia, it's especially grating and troubling!